Imagine waking up each morning with stiff, swollen joints that make it difficult to get out of bed or perform simple tasks like holding a cup or tying your shoes. This is the daily reality for millions of people living with arthritis—a condition that causes chronic pain, inflammation, and stiffness in the joints. Arthritis doesn’t just affect the elderly; it impacts people of all ages, making it a significant health issue worldwide. In this article, we’ll explore the types, causes, symptoms, and treatments of arthritis to help you better understand and manage this common condition.
What Is Arthritis?
Arthritis is not a single disease but a term that encompasses over 100 different conditions that affect the joints and surrounding tissues. The two most common types of arthritis are:
1. Osteoarthritis (OA): A degenerative joint disease that results from wear and tear on the joints, particularly the cartilage that cushions bones. It often affects weight-bearing joints like the knees, hips, and spine but can also impact the hands and feet.
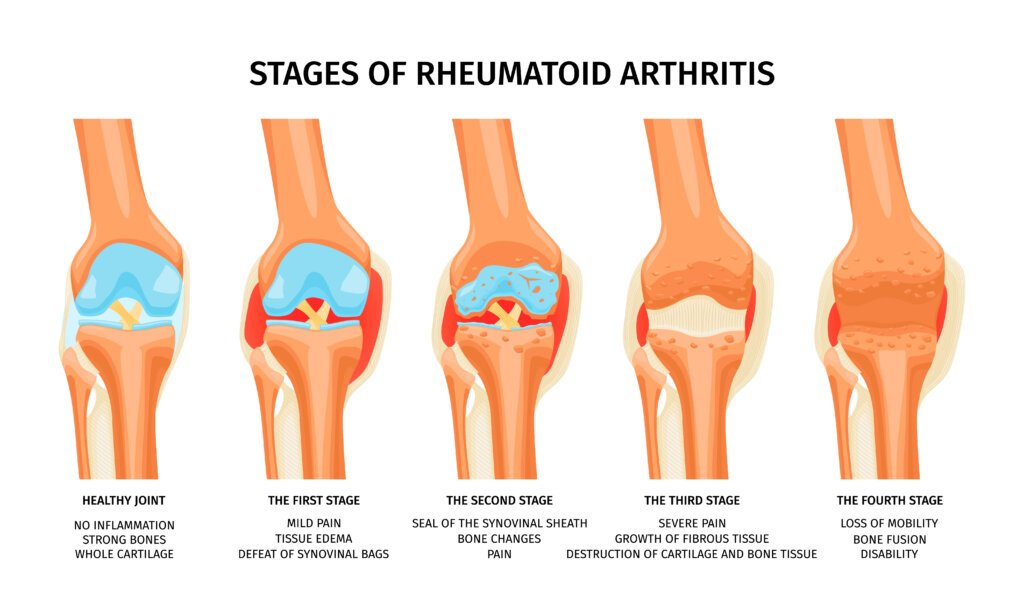
2. Rheumatoid Arthritis (RA): An autoimmune disease where the immune system attacks the synovial membrane surrounding joints, causing inflammation and joint damage. RA can affect multiple joints and may also cause systemic symptoms.
Other forms of arthritis include psoriatic, gout, and juvenile arthritis. Each type has its own unique causes and treatment approaches, but they all share the common symptoms of joint pain and inflammation.
Causes of Arthritis
The causes vary depending on the type, but some common factors include:
1. Aging: As we age, the cartilage in joints can break down, leading to osteoarthritis.
2. Genetics: A family history of arthritis can increase your risk of developing the condition.
3. Autoimmune Disorders: In conditions like rheumatoid arthritis, the immune system mistakenly attacks healthy joint tissues.
4. Injury or Overuse: Repeated stress on joints, whether from physical activity or an injury, can lead to arthritis, especially osteoarthritis.
5. Infections: Certain infections can trigger arthritis, such as in reactive arthritis or septic arthritis.
6. Metabolic Conditions: Conditions like gout, where uric acid builds up in the joints, can also lead to arthritis.
Symptoms of Arthritis
Symptoms vary based on the type and severity of the condition, but common symptoms include:
– Joint Pain: A dull or sharp pain in the affected joints, which may worsen with movement.
– Swelling: Joints may appear swollen or feel tender to the touch.
– Stiffness: Many people with this condition experience stiffness, especially in the morning or after periods of inactivity.
– Reduced Range of Motion: Difficulty moving joints fully or comfortably.
– Warmth or Redness: In some types of arthritis, the joints may feel warm or appear red due to inflammation.
In rheumatoid arthritis, systemic symptoms like fatigue, weight loss, or fever may also be present. In more advanced cases, it can lead to joint deformity and disability.
Diagnosing Arthritis
If you’re experiencing joint pain or stiffness, it’s important to see a healthcare provider for a proper diagnosis. Diagnosing typically involves:
1. Medical History and Physical Examination: Your doctor will ask about your symptoms and check for signs of swelling, warmth, and stiffness in your joints.
2. Imaging Tests: X-rays, MRIs, or ultrasounds may be used to assess the extent of joint damage.
3. Blood Tests: Inflammatory markers (e.g., CRP, ESR) and specific antibodies (e.g., rheumatoid factor) can help diagnose types like rheumatoid arthritis.
4. Joint Aspiration: In cases of gout or septic arthritis, fluid may be drawn from the joint to check for uric acid crystals or infection.
Treatment for Arthritis
While there is no cure for this condition, various treatment options can help manage symptoms and improve quality of life. Treatment approaches depend on the type of arthritis but typically include:
1. Medications:
– Pain Relievers: Over-the-counter pain medications like acetaminophen or NSAIDs (e.g., ibuprofen) can reduce pain and inflammation.
– Disease-Modifying Antirheumatic Drugs (DMARDs): Used in rheumatoid condition to slow disease progression and prevent joint damage.
– Biologics: Targeted therapies that interfere with the immune response, often used in autoimmune arthritis like RA.
– Steroids: Corticosteroids may be prescribed to quickly reduce inflammation.
2. Physical Therapy: Regular exercises that strengthen the muscles around the joints, improve flexibility, and increase range of motion can help relieve symptoms.
3. Lifestyle Modifications:
– Weight Management: Maintaining a healthy weight reduces stress on weight-bearing joints like the hips and knees, lowering your risk.
– Dietary Changes: Anti-inflammatory foods like fish rich in omega-3s, leafy greens, and whole grains may help manage inflammation.
– Low-Impact Exercises: Activities such as swimming, cycling, and walking can help maintain joint mobility without adding excessive stress.
4. Assistive Devices: Braces, canes, or shoe inserts can help reduce joint pressure and make daily activities easier for people with this condition.
5. Surgery: In severe cases where joint damage significantly impacts quality of life, joint replacement surgery (e.g., hip or knee replacement) may be necessary.
Natural Remedies for Arthritis
Some people prefer to complement traditional treatments with natural remedies for arthritis, including:
– Hot and Cold Therapy: Heat can help relax muscles and increase blood flow to the joints, while cold packs can reduce inflammation and numb pain.
– Supplements: Glucosamine, chondroitin, and omega-3 fatty acids may provide relief for some people with osteoarthritis.
– Acupuncture: This ancient practice has shown promise in reducing joint pain and improving function in some studies.
– Massage Therapy: Regular massages can reduce muscle tension, improve circulation, and provide pain relief.
Preventing Arthritis
While some risk factors for arthritis, such as genetics and aging, can’t be changed, there are several steps you can take to lower your risk:
1. Maintain a Healthy Weight: Keeping your weight within a healthy range reduces the strain on your joints, especially your knees, hips, and spine.
2. Stay Active: Regular exercise strengthens the muscles that support your joints, improves flexibility, and helps manage body weight.
3. Protect Your Joints: Use proper body mechanics during physical activities to avoid injury. If you’re lifting heavy objects, be sure to lift with your knees, not your back.
4. Eat a Balanced Diet: A diet rich in fruits, vegetables, lean proteins, and whole grains can help reduce inflammation and promote joint health.
For more information on managing arthritis and improving joint health, consult with a healthcare professional or a rheumatologist.
Missed our last blog? Read about easily breaking bones here
Need health coverage for your Staff? View our Corporate plans here